Why aren’t more doctors prescribing physical activity?
The World Health Organization ranks physical inactivity as the 4th leading risk factor for death worldwide. The need is greater than ever to integrate physical activity into all facets of healthcare. Physical activity can reverse or help manage the symptoms of many chronic conditions, including osteoarthritis which is one of the most common reasons for primary care visits in Canada. Implementation of physical activity prescription within the healthcare profession is part of the World Health Organization’s Global Action Plan on Physical Activity (GAPPA) and is one of ISPAH’s #8Investments that work for physical activity.
Physician-prescribed physical activity is a critical opportunity for helping the one in five inactive Canadian adults meet the physical activity guidelines. A physician’s prescription can increase a patient’s physical activity by 10%. If this was adopted at the population level in Canada, an increase of this level could save $2 billion dollars per year in health care and associated costs. Physical activity prescription by physicians is a cost-effective and underused contribution to this global challenge. A podcast was developed where Dr. Jane Thornton talks about the physical activity prescribing.
BJSM podcast on physical activity prescribing.
Physicians cite lack of time, training and trust as barriers to including physical activity in their counselling practices in the prevention and management of non-communicable disease.
Fundamental training in physical activity prescription is still in its infancy in Canada, particularly as it relates to a treatment strategy. Canadian medical students and residents report the unfortunate juxtaposition of attributing high importance, but having low expertise in physical activity prescription as they complete their training.
Some doctors say that they don’t believe that their patients will engage in physical activity, even if they counselled them to do so. Patients of course face a myriad of barriers to being active that are social, demographic and cultural. These inequalities were highlighted and exacerbated during the COVID-19 pandemic.
We formed the Return to Health and Performance Lab at Western University (London, Canada) to understand more about the barriers and to find solutions that work. Our approach is to increase physician competency and comfort in turning to physical activity for disease prevention and management.
The Return to Health and Performance Lab aims to equip healthcare professionals with evidence-based approaches to using physical activity with their patients through advancing knowledge in how to overcome the three cited barriers.
Time
We have shown that screening patients in advance is highly acceptable for both patient and provider. Also health screening and monitoring via digital health tools can save physicians time while also helping patients achieve their prescribed physical activity level. The Western Research Hub on Physical Activity and Health pulls together a multi-disciplinary team of experts with the aim to save physicians time by studying and communicating best practices on physical activity implementation, to which healthcare providers can signpost instead of searching on their own. This team includes those from Social Sciences, Arts & Humanities, Education and Law and was formed to directly address the GAPPA objectives.
Training
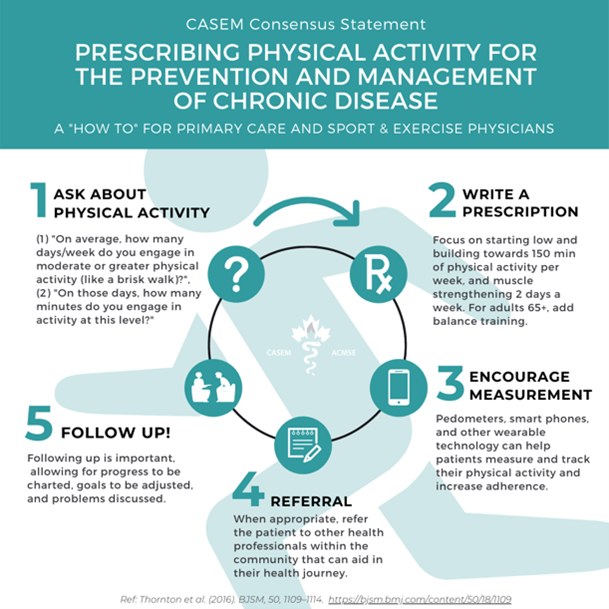
Partnering with the Canadian Academy of Sport and Exercise Medicine (CASEM) has delivered a national strategy to increase and standardize undergraduate medical education on physical activity counselling. In 2016 the Canadian Medical Association adopted our motion to prioritize physical activity in the medical curricula. Our CASEM National Strategy group members have been making steady progress since – physical activity prescription is now in the curriculum of the majority of our 17 medical schools nationwide.
Trust
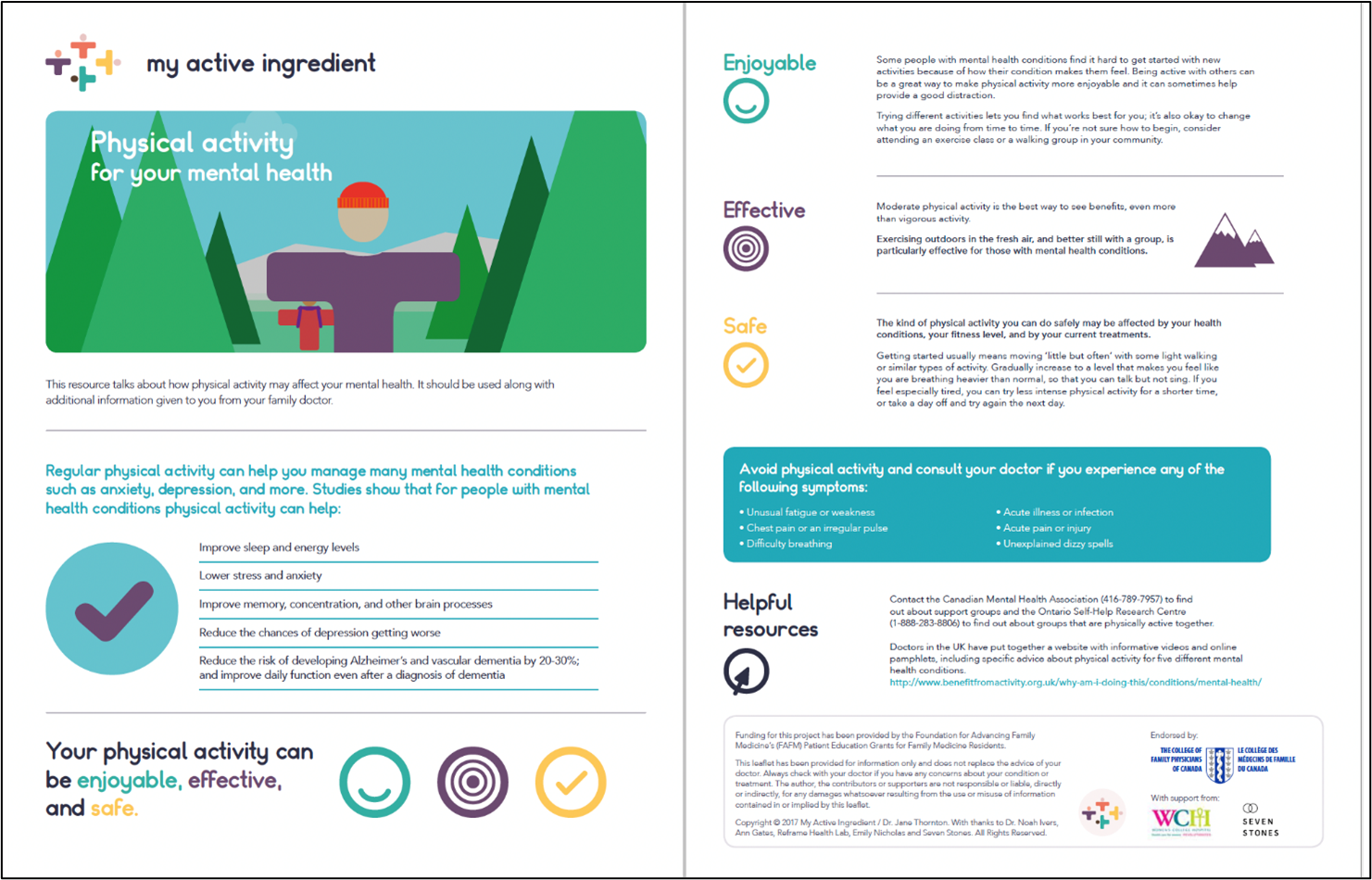
In order to promote engagement of patient groups in the physical activity prescribing agenda we created the “My Active Ingredient” peer-to-peer healthcare hub. The hub is currently active on Twitter through the @myactivingrednt handle and the website is in production. The hub signposts physicians and patients to the best available free physical activity resources. A local Community Advisory Council comprised of patients and community stakeholders inform and co-design interventions. This co-design can maximize potential for effective physical activity interventions in clinical settings. The ultimate aim is to ensure optimal patient outcomes, and advance our understanding of the long-term health-related impacts of physical activity.
Take home messages from our work with physical activity prescription:
- Physicians want to include physical activity into their practices. However, barriers do exist. Training our future doctors and addressing time barriers will help achieve global physical activity goals.
- While healthcare is an important setting for physical activity promotion it is only one of eight of the ISPAH #8investments. Patients have their own barriers too. Healthcare providers must continue to advocate for physical activity across all investments and facilitate access for their patients whenever possible.
- The importance of inter- and multi-disciplinary teams, lived experience, stakeholder involvement is key to advancing successful and sustainable implementation in achieving all of the #8investments.




