Employing practice development techniques to enhances opportunity for change of clinical practice to reduce deconditioning in the acute clinical setting
During hospital admission patients tend to be inactive and highly sedentary. Deconditioning is a common harm related to this, which has long lasting consequences on well-being, independence, physical function and mental health.
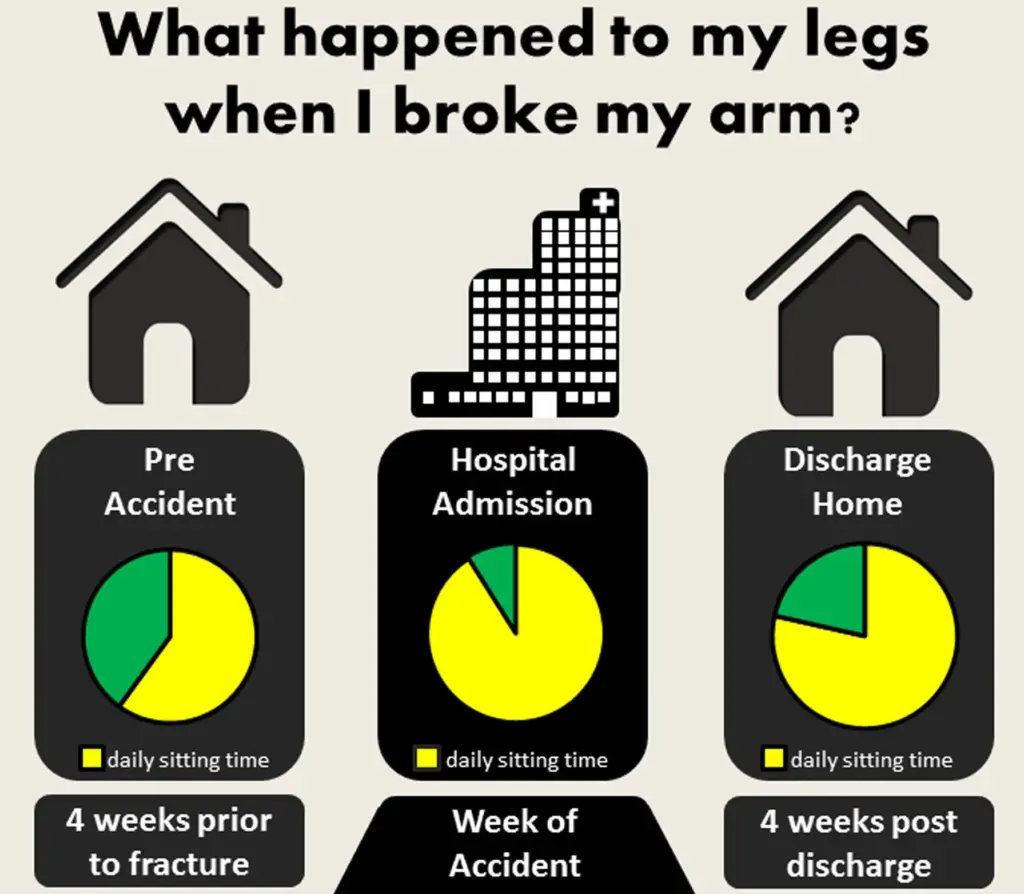
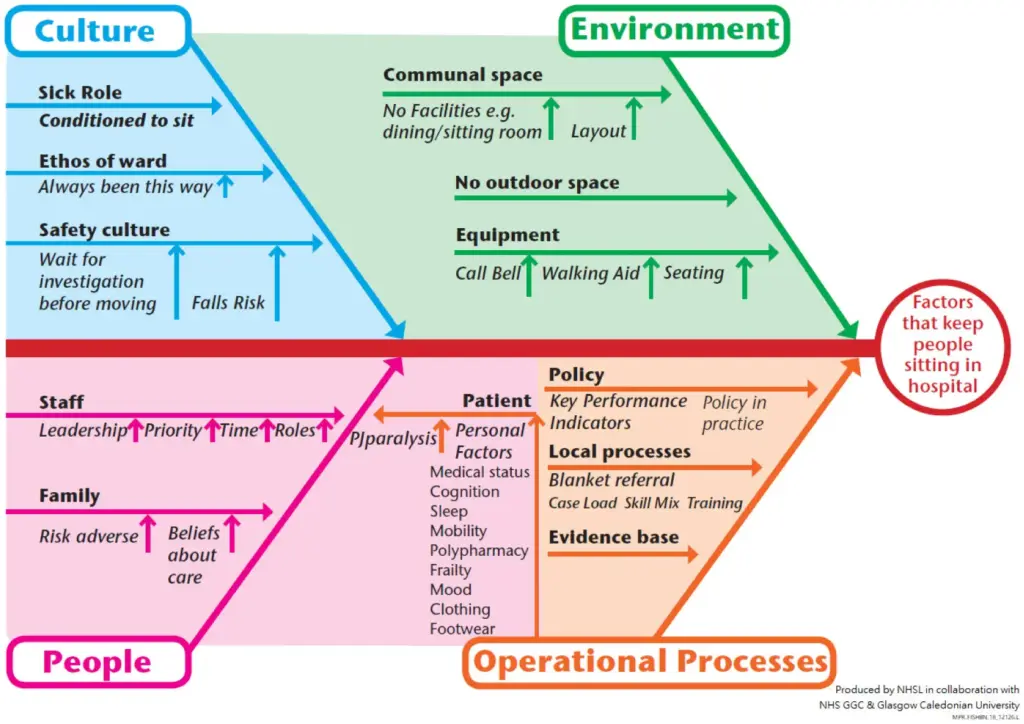
We know patients want to be active during hospital admissions. Many factors influence the risk of deconditioning in hospital relating to the complexity of the organization including culture, the physical environment, people and operational processes as expanded on in the fishbone diagram below. Reducing deconditioning in the clinical environment was considered a priority by Acute Adult Physiotherapy Teams in National Health Service (NHS) Greater Glasgow & Clyde (GGC) Health Board (Glasgow, Scotland). Given the complexity of the issue a holistic view is needed to consider the multiple factors influencing activity behaviour across our diverse clinical settings.
Physiotherapists should feel confident to lead multi-disciplinary efforts to reduce deconditioning in their local specialty. In discussion with Physiotherapy leaders and reviewing results of local staff survey and outputs from development and 4 pillars of practice learning events, it was determined that nearly all physiotherapy staff felt comfortable having discussions with patients about deconditioning, but less were confident in training, leading discussions or instigating change within the broader multi-disciplinary clinical teams in which they work.
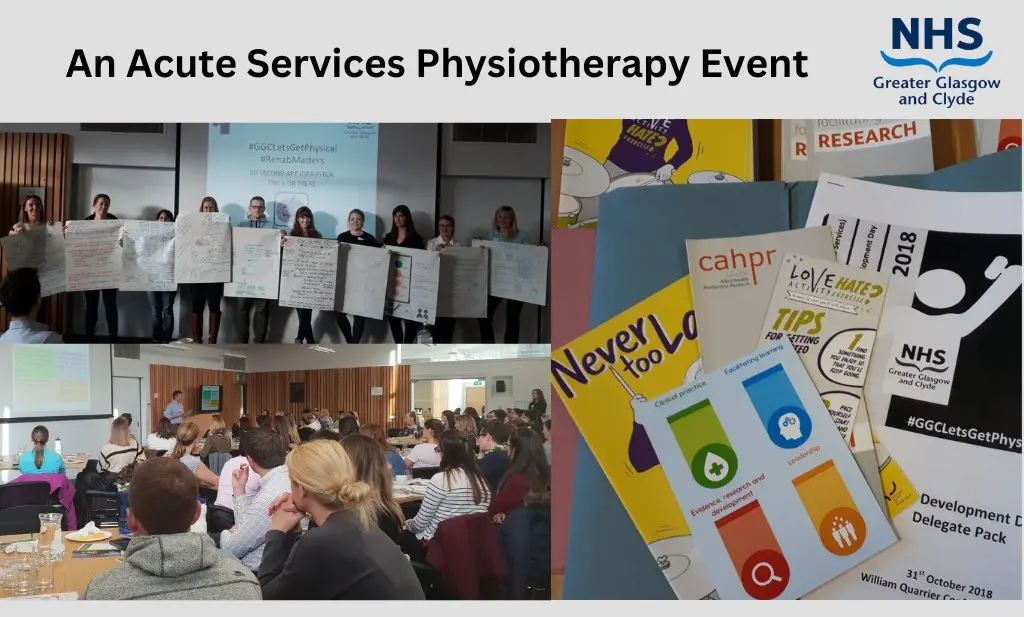
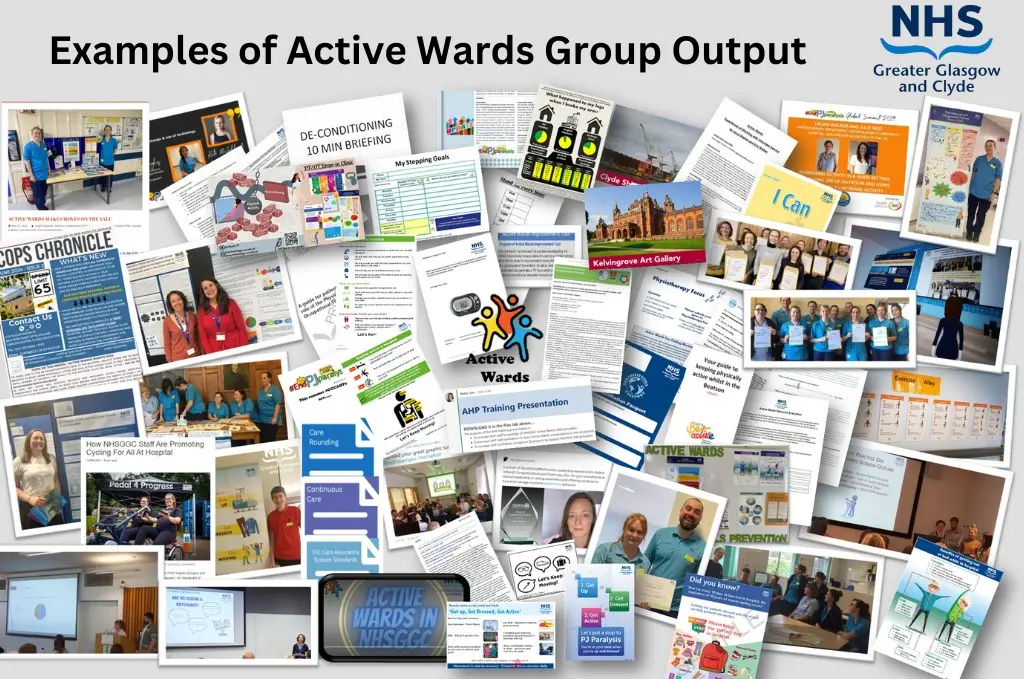
The role of Allied Health Professional (AHP) Practice Development is to facilitate staff development within health services. In 2018, after a period of scoping, examination of the evidence and current provision, the Physiotherapy Practice Development Team were given permission to form a group with representation from across our large health board. It was agreed that these representatives could be released from patient-facing duties to participate in 4-6 meetings/year as well as lead work locally. At this stage, we also invited our Occupational Therapy colleagues to be involved given that both groups work closely to tackle patient activity. The group coined the name “Active Wards” and honed the terms of reference and purpose of the group. The purpose of the group is to increase therapist’s confidence in leading change, provide peer support and act as a platform to share resources and ideas relating to reducing deconditioning in the clinical setting. Group members were from across our health board with therapists and support workers from Older Peoples Services, Stroke, Medical, Surgical, Orthopaedics, Oncology, Critical Care, Neurology, Physical Disability Teams, and rotational staff who change location every 6 months. The group has grown from 18 members in the original group to 52 in 2024. The group use online survey tools and online workspaces to prepare for meetings and communicate between meetings.

The collaborative hub meets in person and online and is where staff network, support each other, conduct projects, share their findings and discuss challenges. They then return to their own team to work on specific quality improvement projects with the ongoing support of the group. Team member reports are completed annually, along with review of the terms of reference. As a result of this participatory collaboration a toolbox of resources were produced for all NHSGGC staff and our Active Wards Principles were co-created.
NHS Greater Glasgow & Clyde Active Wards Principles:
- All patients’ and those involved in their care are supported to understand the benefits of being active in hospital and on discharge.
- We take every opportunity to encourage patients’ to be physically active.
- We minimise environmental barriers to promote physical activity.
- We have a culture where enabling physical activity is everyone’s responsibility.
These principles are now included in guidelines and standards within NHSGGC. The growth of this project has had a ripple effect across NHSGGC and out to other NHS health boards in Scotland. In October 2022 we secured funding for 24-months for one of the group members to join our Practice Development team to dedicate one day per week to taking the active wards work forward by delivery of training and pool our resources. In this post Erin Walker (Specialist Physiotherapist in Older Peoples Services at time of appointment) was awarded the prestigious Sedentary Behaviour Research Network (SBRN) 2023 Practitioner Award and now works as an Advanced Practice Physiotherapist in Frailty. Erin and Juliet continue to co-lead the Active Wards group.
TAKE HOME MESSAGES
- Reducing deconditioning requires holistic consideration of the complexity of the specific needs of each clinical setting.
- Clinicians need adequate time and support to work together with their team to tackle deconditioning in their clinical area.
- Participatory approaches to change are effective in bringing diverse clinical groups together to empower staff to lead change in their local clinical environment and define where efforts can be distributed across the group.
Juliet Harvey, NHS Greater Glasgow & Clyde and University of Dundee, Scotland, UK.




